Исследование микробных загрязнений в контактных линзах и растворах для их консервации
Исследование микробных загрязнений в контактных линзах и растворах для их консервации
Аннотация
Предпосылки: микробный кератит, который может привести к смертельному исходу, является проблемой, связанной с загрязненными контактными линзами и аксессуарами.
Цель настоящего исследования – изучить наиболее распространенные виды бактерий в загрязнениях, связанных с контактными линзами и аксессуарами для ухода за ними, используемыми молодыми людьми, носящими контактные линзы.
Методы: восемнадцать образцов мазков (15 контактных линз и 3 раствора для консервации) были собраны в течение 3 месяцев у разных групп молодых носителей контактных линз. Для первичной идентификации все образцы культивировали на кровяном агаре, агаре МакКонки и декстрозном агаре Сабуру. При положительном росте бактерий проводили каталазный, оксидазный и индольный тесты. Скрининг на 16s рРНК проводили с помощью полимеразной цепной реакции. Диагноз был подтвержден с помощью секвенирования следующего поколения.
Результаты: в данном исследовании процент загрязненных линз составил 60% (9/15), а консервирующего раствора – 66,6% (2/3). Контаминация была представлена в основном бактериями, грибки обнаружены не были. Наиболее распространенными бактериями были Pseudomonas aeruginosa (45,4%) 5 изолятов, затем Achromobacter xylosoxidans (18,1%) два изолята и Rolastenia insidiosa (18,1%) два изолята, наименее загрязненными – Achromobacter pulmoni и Pseudomonas stutzeri с процентом (9%) один изолят для каждого.
Заключение: наше исследование показало, что люди, носящие контактные линзы, не хранят свои линзы и аксессуары для ухода за ними должным образом. Поэтому крайне важно регулярно пересматривать и совершенствовать протоколы использования и ухода за контактными линзами и аксессуарами для них.
1. Introduction
With over 140 million users globally, contact lenses are a popular method of vision correction. Contact lenses are generally well-tolerated, although they can occasionally result in permanent vision loss due to ocular infection (microbial keratitis), with an estimated annualized incidence ranging from ~2 to ~20 cases per 10,000 wearer , . The corneal infection known as microbial keratitis (MK) is a terrible condition that ranks fifth globally in terms of blindness and visual impairment , . A number of characteristics, such as having a professional job as opposed to being a student, replacing contacts once a year as opposed to less frequently, taking daily showers while wearing contacts as opposed to never wearing them, and sleeping in lenses, can raise the risk of contact lens-related microbial keratitis. Most frequently, bacterial keratitis is the cause of MK, which It makes up over 90% of cases; signs and symptoms of bacterial keratitis include photophobia, eyelid swelling, pain, and redness in the eyes , , . Because it is so malicious, pseudomonas is sadly very common in the environment. It is frequently present in water, soil, and normal skin flora. It can flourish in damp and low-oxygen settings in particular, which makes it prone to settle in the confined spaces of medical equipment as well as frequently used objects like sinks and mopsticks . It has been shown that Pseudomonas aeruginosa is the most frequent cause of infections associated with wearing contact lenses .
Gram-negative bacillus Achromobacter xylosoxidans is a member of the Alicaligenes genus. It is frequently mistaken for the Gram-negative bacillus Pseudomonas aeruginosa. a Gram-negative bacillus known as xylosoxidans because of its capacity to oxidize xylose. It is frequently detected by an isolation procedure. Although it is mostly found in soil and water, Achromobacter xylosoxidans can exist in any contaminated environment. Many studies have shown the presence of these organisms in contact lenses. It rarely causes infection in humans, but it has been known to cause opportunistic infections in patients with tumors, hematologic disease, organ transplants, hypogammaglobulinemia, or acquired immunodeficiency syndrome (AIDS) , , . So, the aim of current study to examine the most prevalence bacteria species in the contaminants associated with contact lenses.
2. Methods
2.1. Sample collection and culturing
eighteen samples (15 contact lenses and 3 conservation solution) were collected for 3 months, all personal information about (age, wearing history, handling and cleaning process) were recorded, all participates in the current study were females since no male subject had been encountered wearing contact lens during the study period.
Collected sample were labelled, for primary microbial isolation and identification, all samples were cultured on the blood agar, MacConkey agar sabouraud dextrose agar, incubated for 24-48 hours. Colonial morphology such as (shape, texture, size) as well as hemolysis, pigments, odor were recorded in addition to biochemical tests (Indole, oxidase and catalase) were done.
2.2. Polymerase chain reaction
To extract DNA from bacteria, the purification Wizard genomic DNA kit was utilized. According to the manufacturer's recommendations, bacterial growth was cultured overnight on Lauryl Broth (LB) at 37°C for 24 hours. After that, the growth was transferred to Eppendorf tubes and centrifuged at 1300 rpm for 3 minutes before extraction. PCR was carried out using a particular primer set in order to find and identify the genes in the DNA that was isolated from bacteria. The procedure for PCR amplification is shown in Table 1.
Table 1 - Primer sequence
Genes | Sequence | PCR Product/bp | Tm | References |
16s RNA | 27F -`AGAGTTTGATCCTGGCTCAG 1492R -TACGGTTACCTTGTTACGACTT | 1500 | 30sec. at 60 C˚ | 12 |
Note: PCR products were electrophoresed in 1.5% agarose gel
2.3. Gene Analysis
Macrogen Corporation-Korea provided the results of the PCR of 16 sRNA for the Sanger sequence utilizing an automated DNA sequencer, the ABI3730XL. After receiving the results via email, Geneious software was used for analysis .
3. Results
Every participant followed proper CL care procedures, which included checking the expiration dates of the CL product and solution, inspecting the side of the lens, washing their hands with soap before putting the CL in and taking it out, and changing the cleaning solution once a month.
Out of 18 collected sample 11 were contaminated with different types of bacteria, all microbial contaminate isolated were bacteria; but no fungi were found. While new and unused contact lens and solutions don’t have any contamination. The percentage of contaminate lenses was 60% (9/15) while preservation solution 66.6% (2/3). The most prevalence bacteria were Pseudomonas aeruginosa (45.4%) 5 isolates followed by Achromobacter xylosoxidans (18.1%) two isolates and Rolastenia insidiosa (18.1%) two isolates, the least contaminants are Achromobacter pulmoni and Pseudomonas stutzeri with percentage (9%) one isolate for each.
The information of age, contact lens wearing history, Number of times contact lenses are used, and isolated bacteria in figure 1,2 and table 2.
Table 2 - The information contact lenses and isolated bacteria
Subject ID | Age | Wearing history | Number of times used | Result |
CL-1 | 26 | 3 months | Four times | No growth |
CL-2 | 28 | One year | Six times | No growth |
CL-3 | 26 | One year | One time | Achrmobacter xylosoxidans |
CL-4 | 20 | More than one year | Six times | Pseudomonas aeruginosa |
CL-5 | 30 | One year | One time | Pseudomonas aeruginosa |
CL-6 | 21 | One year | Three times | Achrmobacter xylosoxidans |
CL-7 | 27 | 2 months | Four times | No growth |
CL-8 | 29 | 2 months | Three times | No growth |
CL-9 | 30 | 2 month | Six times | Pseudomonas aeruginosa |
CL-10 | 30 | Month | Four times | Pseudomonas stutzeri |
CL-11 | 34 | 5 months | Three times | No growth |
CL-12 | 32 | 2 months | Two times | Ralstonia insidiosa |
CL-13 | 34 | Not opened | Non -user | No growth |
CL-14 | 36 | 2 month | Four times | Pseudomonas aeruginosa |
CL-15 | 38 | 4 month | Sixth times | Pseudomonas aeruginosa |
C-16 | 33 | 5 months | Three times | Achromobacter pulmonis |
C-17 | 30 | 2 months | Two times | Ralstonia insidiosa |
C-18 | - | Not opened | Non -user | No growth |
Note: contct lens; C: conservative solution
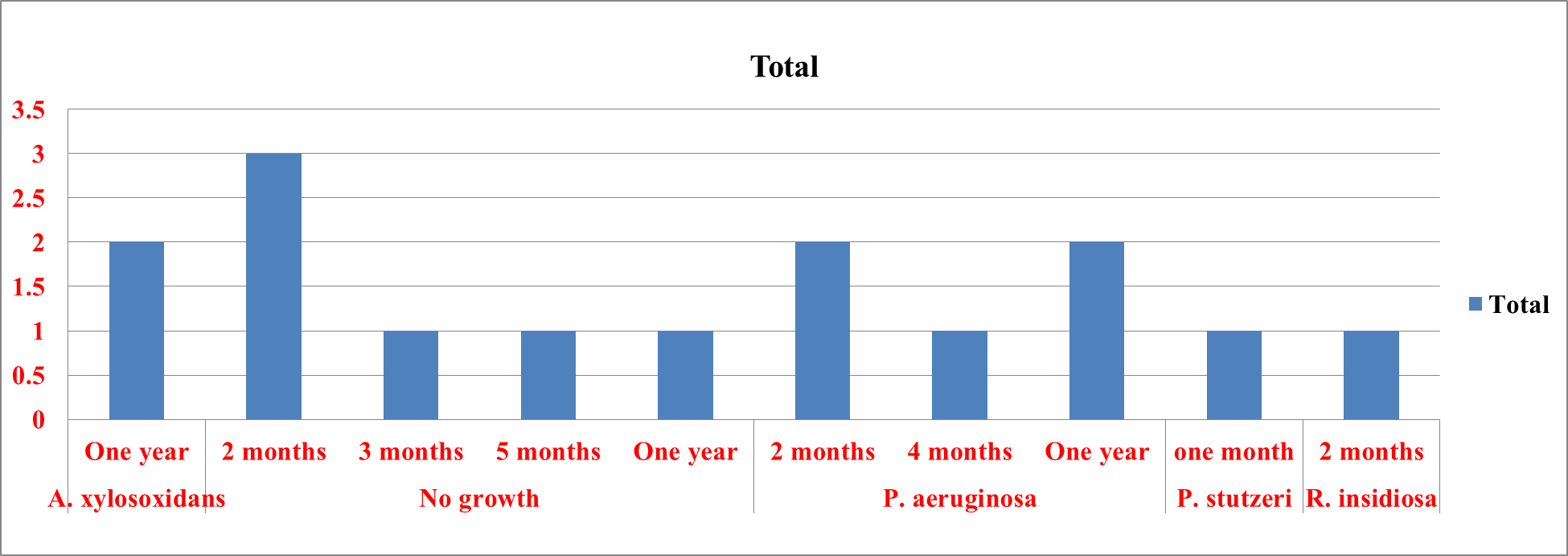
Figure 1 - Bacterial growth in contact lenses
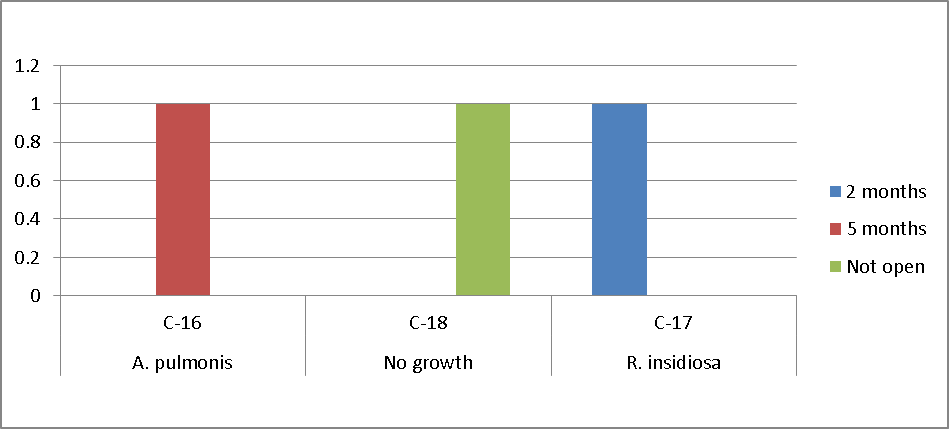
Figure 2 - Bacterial growth on preservation solution
Table 3 - Nucleotide details of each bacteria both strand
Bacterial isolates | Content of G, A, C, T in reverse strand | Content of G, A, C, T foreward strand | ||||||
A, % | C, % | G, % | T, % | A, % | C, % | G, % | T, % | |
Achromobacter pulmonis | 16.51 | 15.5 | 41.9 | 26.04 | 17.2 | 20.06 | 40.2 | 22.54 |
Ralstonia insidiosa | 26.49 | 24.05 | 32.7 | 6.76 | 28.04 | 25.32 | 31.73 | 14.9 |
Achromobacter xylosoxidans | 22.82 | 22.82 | 30.99 | 23.38 | 22.95 | 20.0 | 30.26 | 26.79 |
Pseudomonas aeruginosa | 17.1 | 14.33 | 41.79 | 26.79 | 30.33 | 20.33 | 28.67 | 20.67 |
Pseudomonas aeruginosa | 21.36 419 | 19.37 380 | 33.33 654 | 25.94 509 | 29.02 | 23.61 | 25.2 | 22.16 |
Pseudomonas aeruginosa | 26.19 | 19.23 | 30.95 | 23.63 | 28.0 | 31.81 | 20.57 | 19.62 |
Achromobacter xylosoxidans | 16.74 | 15.2 | 42.63 | 25.43 | 24.49 | 25.75 | 28.28 | 21.48 |
Pseudomonas aeruginosa | 23.82 | 21.21 | 30.21 | 24.76 | 21.56 | 24.94 | 26.75 | 26.75 |
Pseudomonas aeruginosa | 23.1 | 23.1 | 26.2 | 27.61 | 19.77 | 31.4 | 27.13 | 21.71 |
Pseudomonas stutzeri | 20.07 | 29.23 | 27.46 | 23.24 | 18.64 | 27.96 | 29.22 | 24.18 |
Ralstonia insidiosa | 25.16 | 25.16 | 29.03 | 20.65 | 32.08 | 20.91 | 23.09 | 23.91 |
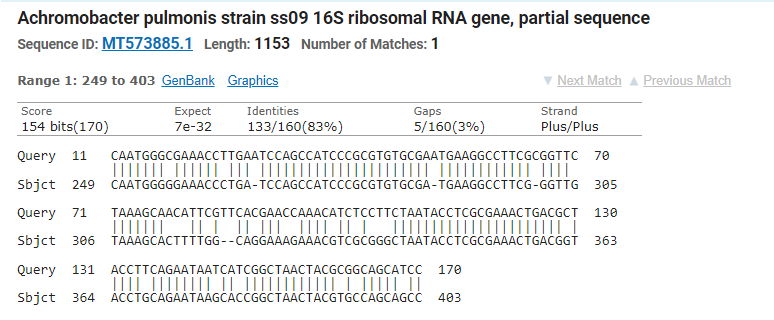
Figure 3 - Achromobacter pulmonis strain ss09 16S ribosomal RNA gene, partial sequence
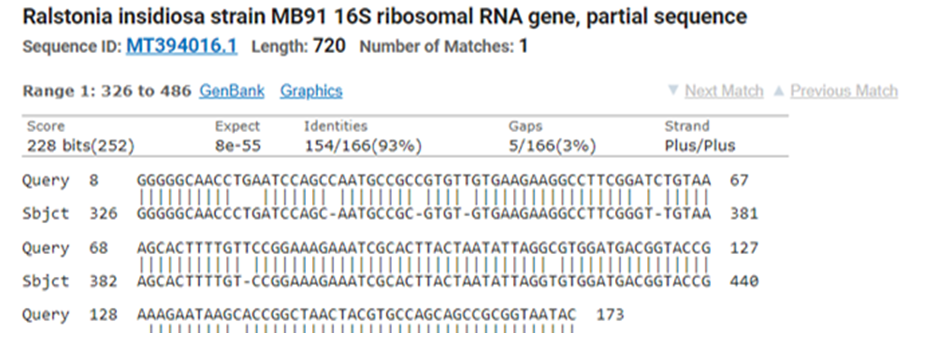
Figure 4 - Ralstonia insidiosa strain MB91 16S ribosomal RNA gene, partial sequence
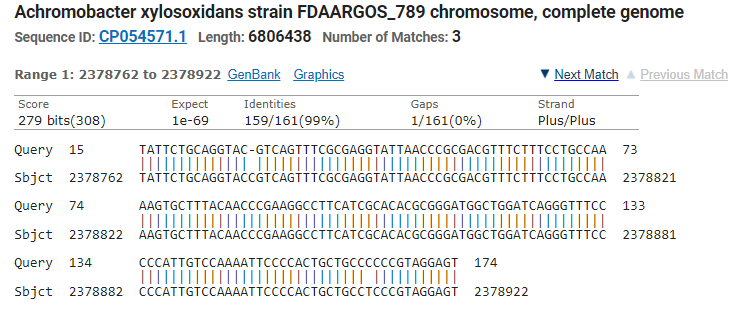
Figure 5 - Achromobacter xylosoxidans strain FDAARGOS_789 chromosome, complete genome
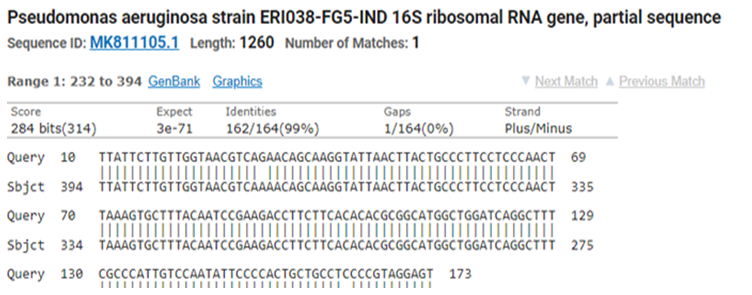
Figure 6 - Pseudomonas aeruginosa strain ERI038-FG5-IND 16S ribosomal RNA gene, partial sequence
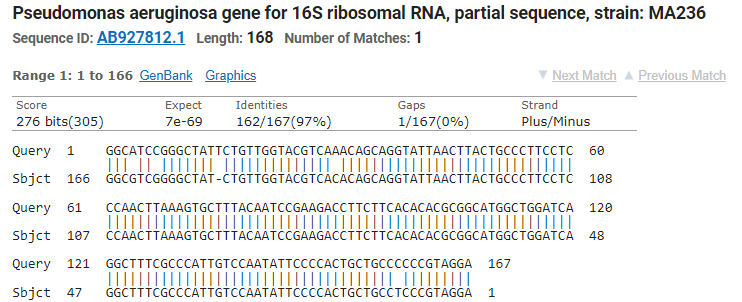
Figure 7 - Pseudomonas aeruginosa gene for 16S ribosomal RNA, partial sequence, strain: MA236
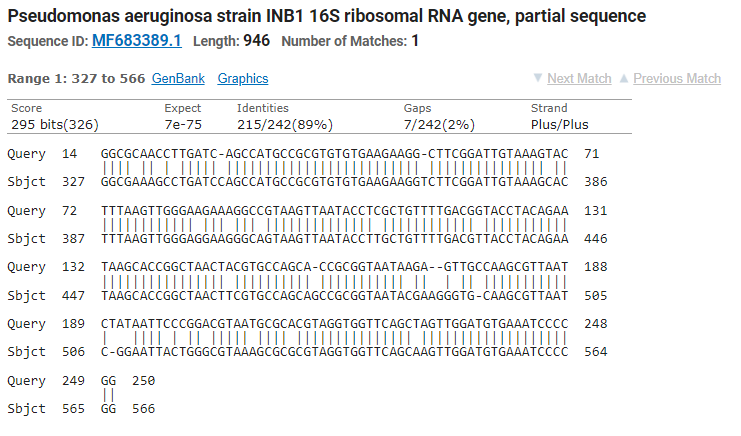
Figure 8 - Pseudomonas aeruginosa strain INB1 16S ribosomal RNA gene, partial sequence
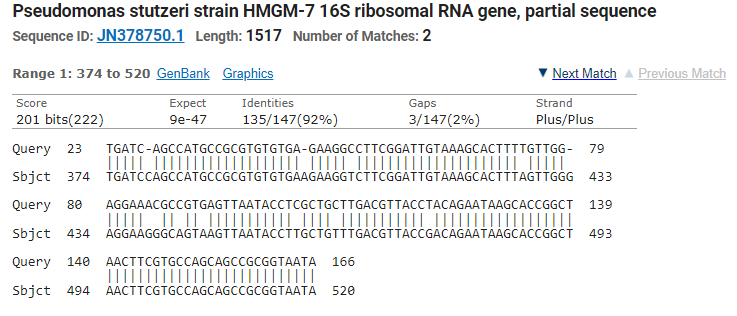
Figure 9 - Pseudomonas stutzeri strain HMGM-7 16S ribosomal RNA gene, partial sequence
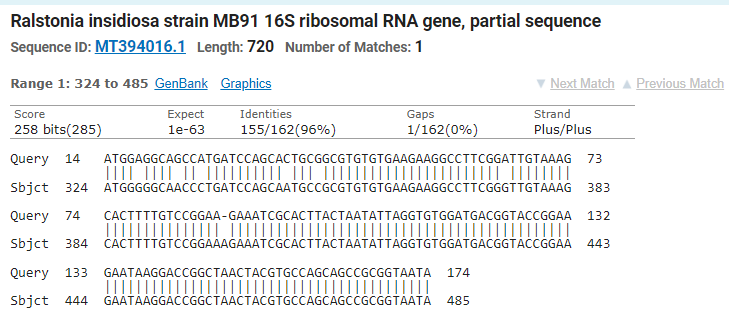
Figure 10 - Ralstonia insidiosa strain MB91 16S ribosomal RNA gene, partial sequence
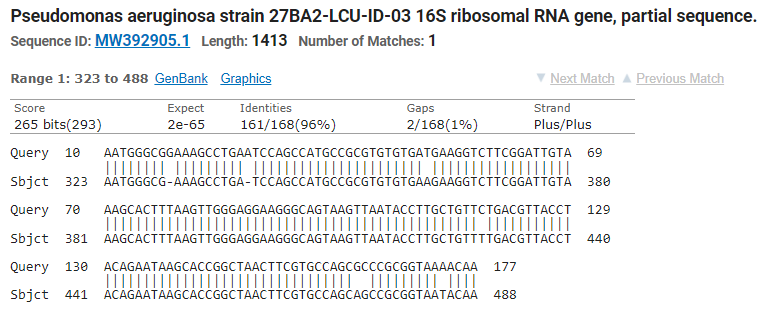
Figure 11 - Pseudomonas aeruginosa strain 27BA2-LCU-ID-03 16S ribosomal RNA gene, partial sequence
4. Discussion
It has been suggested that the usage of contaminated cleaning solutions and contact lenses is linked to the development of keratitis. Particularly when handled incorrectly, certain microorganisms have the potential to stick to the surface of contact lenses, colonize the cornea while being used, and live in the lens case . As the water content of a contact lens decreases, bacterial adhesion to the lens is known to increase, and hydrophobic lenses are more prone to bacterial adherence than high water-content lenses . It is crucial to note that the contact lenses were purchased from a separate commercial company, which helps to explain why certain opening lenses do not become contaminated with germs even after a year of use.
Since all of the contact lenses that were cultured were soaked in conservation solution, it is possible that microorganisms first thrived in the lens case before secondary contamination of the lens occurred. This makes the lens cases stationary, which is better for the formation of biofilm than contact lenses.
Biofilm on the case surface offers sites for additional microorganisms to adhere to and shields bacteria from disinfectants physically . In addition, contact lenses left in their cases for extended periods of time without being used create an environment that is more conducive to microorganism attachment and biofilm accumulation.
In the contaminated conservation solution, two distinct types of bacteria were discovered. Even so, it's made to serve a variety of functions, such as washing, rinsing, and storing contact lenses. Contamination is typically related to handling since, even though solutions contain disinfectant, contact lens wearers typically pay more attention to lens hygiene than solution hygiene. As a result, solutions are more likely to become contaminated. Additionally, during solution storage, antimicrobial activity may decrease. Additionally, some organisms may be able to use the chemicals in lens solutions as nutrition, but saline would not be able to give such nutrients. This means that handling techniques need to be improved, and the significance of replacing opening lens care solutions on a frequent basis needs to be emphasized.
These outcomes could be caused by the fact that handling lenses while unclean can transfer germs from the nails, skin, and even the air, particularly after coming into touch with contaminated surfaces, water, or dirt. The germs can live in improperly maintained storage containers or in dirty contact lens cases. Cosmetics, particularly mascara and eye shadow, can spread infection, particularly when applied with unclean applicators or because Contamination can be increased by sharing lens care products or cases, using Extended Wear lenses, which are more likely to become contaminated because they are in the eye for extended periods of time, and handling lenses improperly, which includes rubbing, rinsing too much, or failing to disinfect thoroughly.
According to a 2007 study, 9%, 11%, and 13%, respectively, of contact lenses and conservative solutions were contaminated . According to available data, Pseudomonas aeruginosa is the most frequent cause of infections linked to contact lens usage . According to recent research, contact lens solutions, lens cases, and lenses can all become contaminated by Achromobacter spp., which can then lead to corneal infiltrative events (CIEs) , , . A study conducted by Udomwech et al. in 2022 shows that 17.41%, 10%, and 5% of contact lenses were contaminated with Acromobacter, Pseudomonas aeruginosa, and Pseudomonas stutzeri, respectively. The types and amounts of microbial contamination that can occur from different cleaning solutions used during lens storage can vary, with certain solutions exhibiting higher rates of contamination by specific microorganisms, including as Gram-negative bacteria .
5. Conclusion
In Iraq, where access to hygienic facilities and clean water may be restricted, contact lens contamination by bacteria continues to be a serious public health concern. The danger of contamination is increased by environmental conditions, inadequate care, and poor hygiene practices. It is possible to minimize the risk of eye infections and ensure the safety and comfort of millions of contact lens wearers worldwide by implementing customized preventive measures based on an understanding of the sources of contamination and the specific bacteria that are common in contact lenses. Using sterile solutions, washing your hands properly, and scheduling routine eye exams are all important preventive actions that help lower the risk of contact lens contamination. Our findings also indicate that novel techniques for shielding contact lenses and lens care supplies from impurities are required. These could include new materials for contact lenses or lens cases that are resistant to microbe attachment, as well as adjusted lens care solutions with stronger antibacterial agents.
Larger population-based studies are advised in order to determine and validate the link between specific unsanitary habits and CL wear, as well as to inform the general public — and soft CL wearers specifically — about the risk of serious microbial infections that may arise from high contamination rates brought on by unsanitary habits.